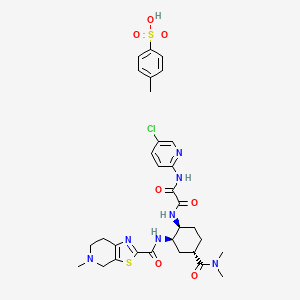
Edoxaban Tosylate: Usage, Side Effects, Precautions
Edoxaban Tosylate belongs to a group of medicines called anticoagulants, also known as blood thinners.
This drug prevents the formation of blood clots by blocking factor Xa, an important substance that helps blood to clot.
It is used in adults to prevent the formation of blood clots in the brain (stroke) and other vessels of the body in patients with an irregular heartbeat called non-valvular atrial fibrillation and at least one additional risk factor.
It is used to treat blood types in the veins of the legs (deep vein thrombosis) and blood vessels (Pulmonary embolism) and to prevent the recurrence of blood clots in the blood vessels of the legs and/or lungs.
What Will We Learn?
Before You Use Edoxaban Tosylate
Do not use Edoxaban tosylate in the following cases:
- If you are allergic to edoxaban or any ingredient in this medicine.
- if you have excessive bleeding
- if you have a disease that increases the risk of serious bleeding from an organ in your body (such as a stomach ulcer, recent brain hemorrhage or damage, or recent brain or eye surgery)
- If you are taking other medicines that prevent blood clots (eg, warfarin, dabigatran, rivaroxaban, apixaban, or heparin) (except when changing your anticoagulant therapy and using heparin to keep the vein or capillary line open)
- If you have a liver disease that increases the risk of bleeding
- If you have uncontrollable high blood pressure
- If you are pregnant or breastfeeding
Use edoxaban tosylate with caution in the following situations:
Consult your doctor or pharmacist before using Edoxaban tosylate in the following situations.
If you have an increased risk of bleeding, which is if you have any of the following conditions:
- End-stage kidney disease or dependence on dialysis
- Serious liver disease
- Bleeding disorders
- Problem with the blood vessels at the back of the eye (retinopathy)
- Recent cerebral hemorrhage (intracranial or intracerebral hemorrhage)
- Problems with blood vessels in the brain or spinal cord
- If you have a mechanical heart valve
Tell your doctor if you know you have a disease called antiphospholipid syndrome (an immune system disease that increases the risk of blood clots forming).
Your doctor will decide if your treatment needs to be changed.
If you are going to have an operation, it is very important that you use edoxaban tosylate before and after the operation in accordance with the hours specified by your doctor.
If possible, stop using edoxaban tosylate at least 24 hours before surgery.
Your doctor will decide when to start using edoxaban tosylate again. In an emergency, your doctor will assist you in determining appropriate actions regarding Edoxaban tosylate.
Pregnancy And Breastfeeding
Consult your doctor or pharmacist before using this medication.
Do not use Edoxaban tosylate if you are pregnant.
If you can become pregnant, you should use a reliable method of contraception while using edoxaban tosylate.
If you become pregnant while using edoxaban tosylate, consult your doctor immediately.
Your doctor will decide whether to continue treatment.
If you find out that you are pregnant during your treatment, consult your doctor or pharmacist immediately.
Do not use Edoxaban Tosylate if you are breastfeeding.
Other drugs and Edoxaban tosylate
Please inform your doctor or pharmacist if you have the possibility to use any medicine, if you are using it now or if you have used it recently.
In particular, inform your doctor about this if you are using any of the following drugs:
- Some medicines for fungal infections (eg ketoconazole)
- Medicines used to treat abnormal heartbeats (eg dronedarone, quinidine, verapamil)
- Other medicines used to prevent blood clots (eg heparin, clopidogrel or vitamin K antagonists such as warfarin, acenocoumarol, phenprocoumon, or dabigatran, rivaroxaban, apixaban)
- Antibiotic drugs (eg erythromycin)
- Medicines used to prevent the body from rejecting the organ after an organ transplant (eg cyclosporine)
- Anti-inflammatory and pain medications (eg naproxen or acetylsalicylic acid (aspirin)).
- Antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs)
If any of the above apply to you, inform your doctor before you start using this medicine because these medicines may increase the effect of Edoxaban tosylate and cause unwanted bleeding.
Your doctor will decide whether you should be treated and observed with Edoxaban tosylate.
Inform your doctor if you are using any of the medicines listed below, as these may reduce the effect of Edoxaban tosylate.
- Some drugs used to treat epilepsy (eg phenytoin, carbamazepine, phenobarbital)
- St John’s Wort, herbal supplement used for restlessness and mild depression
- Rifampicin, an antibiotic
Your doctor will decide whether you should be treated and observed with Edoxaban tosylate.
If you are currently using or have recently used any prescription or non-prescription drugs, please inform your doctor or pharmacist about them.
How To Use Edoxaban Tosylate?
Always take your medicine exactly as your doctor has told you. If you are not sure, check with your doctor.
Medications containing the Edoxaban Tosylate ingredient usually come in same-sized tablets, but there may be exceptions.
Please note that your doctor will give your best advice, not this article. Contact your doctor if you have questions about use.
The recommended dose is one 60 mg tablet once a day.
- If you have impaired kidney function, the daily dose can be reduced to one 30 mg tablet once a day by your doctor.
- If your body weight is 60 kg or less, the recommended daily dose is one 30 mg tablet once a day.
- If your doctor has prescribed you a medicine known as a P-gp inhibitor (cyclosporine, dronedarone, erythromycin or ketoconazole): the recommended daily dose is one 30 mg tablet once a day
Your doctor may change your anticoagulant therapy as follows:
- Switching from anticoagulant therapy containing a vitamin K antagonist (e.g. warfarin) to edoxaban tosylate: Stop taking anticoagulant medication containing a vitamin K antagonist (e.g. warfarin). Your doctor will need to take blood measurements and will tell you when you should start using edoxaban tosylate.
- Switching from non-VKA (vitamin K antagonist) oral anticoagulants (dabigatran, rivaroxaban or apixaban) to edoxaban tosylate: Stop using previous medications (eg dabigatran, rivaroxaban or apixaban) and start treatment with edoxaban tosylate at the time you should take the next scheduled dose.
- Switching from parenteral anticoagulant drugs (eg heparin) to edoxaban tosylate: Stop using the anticoagulant medication (eg heparin) and start treatment with edoxaban tosylate at the time you need to take the next scheduled dose of anticoagulant.
- Switching from edoxaban tosylate to anticoagulant therapy containing a vitamin K antagonist (e.g. warfarin): If you are using edoxaban tosylate 60 mg: Your doctor will reduce your dose of edoxaban tosylate to 30 mg tablets per day and will tell you to take it with a vitamin K antagonist-containing medicine (e.g. warfarin). . Your doctor will need to take blood measurements and will tell you when to stop using edoxaban tosylate.
- If you are using (reduced dose) edoxaban tosylate 30 mg: your doctor will reduce your dose of edoxaban tosylate to 15 mg tablets per day and tell you to take it with a medicine containing a vitamin K antagonist (eg warfarin). Your doctor will need to take blood measurements and will tell you when to stop using edoxaban tosylate.
- Switching from edoxaban tosylate to non-VKA (vitamin K antagonist) oral anticoagulants (dabigatran, rivaroxaban or apixaban). Stop using edoxaban tosylate and start treatment with a non-VKA oral anticoagulant drug (eg dabigatran, rivaroxaban, or apixaban) at the time you should take the next scheduled dose of edoxaban tosylate.
- Switching from edoxaban tosylate to parenteral anticoagulant drugs (eg heparin). Stop using edoxaban tosylate and start treatment with a parenteral anticoagulant drug (eg heparin) at the time you should take the next scheduled dose of edoxaban tosylate.
If your abnormal heartbeat needs to return to normal with a process called cardioversion, take edoxaban tosylate as recommended by your doctor to prevent blood clots that may form in your brain and other blood vessels in your body.
Edoxaban tosylate should be swallowed whole, with or without food, with some water.
If you have trouble swallowing the tablet whole, talk to your doctor about other ways to take this medicine.
The tablet can be crushed and mixed with water or applesauce just before use.
If necessary, your doctor may also give you a crushed edoxaban tosylate tablet through a stomach tube.
Edoxaban tosylate is not recommended for children and adolescents under 18 years of age.
There is no information available on its use in children and adolescents.
You should not use this medicine if you are a patient with end-stage renal disease or dialysis.
The recommended dose for patients with mild renal impairment is 60 mg per day.
The recommended dose of edoxaban tosylate for patients with moderate or severe renal impairment is 30 mg per day.
If your liver enzymes are more than twice the normal level, the use of this drug is not recommended.
The use of this drug is not recommended in patients with severe hepatic impairment.
The recommended dose for patients with mild to moderate hepatic impairment is 60 mg.
This drug should be used with caution in patients with mild to moderate hepatic impairment.
Edoxaban tosylate should not be used in patients with liver disease that may cause bleeding risk.
If you have the impression that the effect of the medicine is too strong or too weak, talk to your doctor or pharmacist.
Side Effects Of Edoxaban Tosylate
Like all medicines, side effects may occur in people who are sensitive to the ingredients of this medicine.
As with other similar drugs (blood clotting inhibitors), the use of this drug can cause life-threatening bleeding.
Sometimes these bleedings may not be clearly understood.
If any of the side effects listed below occur, stop using edoxaban tosylate and tell your doctor immediately or go to the nearest hospital emergency department:
Unusual:
- Hypersensitivity (hypersensitivity reactions)
Rare:
- Anaphylactic reaction
- Allergic edema
These are all very serious side effects. If you have one of these, you are allergic to edoxaban tosylate. You may need emergency medical attention or hospitalization.
If you experience episodes of bleeding that does not go away on its own, or if you experience signs of excessive bleeding (extreme weakness, tiredness, paleness, dizziness, headache, and unexplained swelling), consult your doctor immediately.
All these are serious side effects.
Emergency medical attention may be required.
Your doctor may keep you under closer observation or change your treatment.
Common side effects are listed below:
- Stomach ache
- Abnormal liver blood tests
- Bleeding from the skin or under the skin
- Anemia (low level of red blood cells)
- Nose bleeding
- Bleeding from the vagina
- Bleeding in the gut
- Bleeding from the mouth and/or throat
- Seeing blood in the urine
- Bleeding after injury (bleeding at the puncture site)
- Nausea
- Stomach bleeding
- Dizziness
- Don’t feel sick
- Headache
- Itching
- Increase in bilirubin (a substance normally found in the liver) in the blood
- Increase in gamma-glutamyl transferase (an enzyme found in many organs in the body and in the liver)
- Redness
- Bleeding in the eyes (conjunctival/scleral hemorrhage, intraocular hemorrhage)
- Post-operative bleeding from the surgical wound
- Coughing up blood
- Cerebral hemorrhage
- Other types of bleeding
- Decreased platelet count in the blood (which may affect clotting)
- Allergic reaction
- Hives
- Increase in the level of alkaline phosphatase (an enzyme that is intensely produced in our body, especially in the skeletal system and gastrointestinal tract) in the blood
- Increase in the level of transaminases (a type of liver enzyme) in the blood
- Bleeding in the muscles
- Intra-articular bleeding
- Intra-abdominal bleeding (retroperitoneal hemorrhage)
- Bleeding in the heart
- Intracranial hemorrhage (subarachnoid hemorrhage, subdural hemorrhage)
- Post-surgical bleeding
- Allergic shock
- Swelling in any part of the body due to an allergic reaction
If any of the side effects listed above occur, contact your doctor without waiting.
It should be noted that the side effects listed above are not a complete list, and if you experience any different effects, inform your doctor about this.
Our article on Paricalcitol may also attract your attention.
