What Is Urinary Incontinence? How Is It Treated?
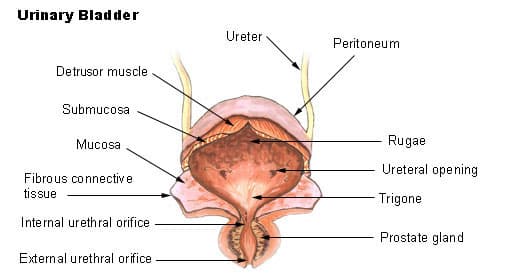
The bladder, known as the urinary bladder, refers to the sac where urine from the kidneys is collected.
While the contraction and relaxation of the bladder muscles are controlled by the nerves in that area and the brain, the muscles at the lower end of the bladder, which stretch as the urine is filled, keep the mouth of the pouch closed.
Urinary incontinence is the uncontrollable and involuntary leakage of urine.
Although it can occur at any age, urinary incontinence, which is more common in older ages, is considered a disease if it is repeated continuously.
This disorder, which seriously affects the quality of life, is more common especially in women.
What Will We Learn?
What Causes Incontinence?
With aging, the functions of the muscles that function to empty the urine only when desired may decrease.
However, there may be other reasons as well.
For example, diseases such as diabetes can be effective in urinary incontinence.
Apart from this, diseases that may affect the central nervous system such as stroke and spinal cord injury and that may adversely affect the peripheral nervous system such as nerve injuries can also cause this disorder.
We can list the risk factors that can lead to urinary incontinence and the causes of this discomfort in general as follows:
- Being overweight
- Asthma etc. diseases
- Smoking
- Chronic cough and constipation
- Fistula between vagina and bladder
- Genetic factors
- Bladder prolapse
- Intra-abdominal pressure seen in heavy workers
- Advancing age
- Cystitis
- Vaginal infections
- Diabetes
- Menopause
- Prostate enlargement in men
- Nervous system diseases
- Dementia Alzheimer’s disease
- Stone formed in the urinary tract or kidney
- Muscle relaxants, diuretics, blood pressure lowering, tranquilizers, antidepressants.
Apart from these, muscle rupture and nerve damage may occur in difficult births. It is known that this situation leads to dysfunctions.
In addition, the causes of urinary incontinence can be divided into two subheadings as temporary and chronic:
Temporary Urinary Incontinence Causes
- Clouding of consciousness
- Urinary tract infection
- Vaginal and urethra estrogen deficiency
- Medicines
- Psychiatric reasons
- Excessive urination
- Limitation of movement
Causes of Chronic Urinary Incontinence
- Stress incontinence
- Urge incontinence
- Overflow incontinence
- Mixed incontinence
What Causes Incontinence In Men?
Incontinence, which is less common in men than in women, can result from an overactive bladder.
In addition, it usually occurs during stressful physical exertion such as sneezing, coughing, or due to a strong and sudden urge to urinate.
What Causes Incontinence In Women?
Urinary bladder sagging and menopause due to difficult births are the main causes of urinary incontinence in women.
In addition to these, giving birth to excess is one of these reasons.
Urinary incontinence, which can be seen even in women who have never given birth, is shown as a hereditary disorder.
What Are The Symptoms Of Urinary Incontinence?
We can list the symptoms of urinary incontinence, which can start with the involuntary drip or sudden leakage of urine, as follows:
- Frequent urge to urinate
- Painful urination without any bladder infection
- Inability to urinate
- Common bladder infections
What Are The Types Of Urinary Incontinence?
Urinary incontinence is divided into two types, transient and chronic.
Temporary incontinence does not repeat as it can be understood from the name.
After the reasons for the discomfort are treated, the patient does not miss the urine again.
These people do not have any anatomical or neurological problems in their urinary tract.
People with chronic urinary incontinence have a problem in their urinary tract.
Apart from these, there are also types such as urge incontinence, stress incontinence and continuous urticaria incontinence.
- Stress Incontinence: It is the state of urinary incontinence in situations where the pressure in the urinary bladder increases, such as laughing, sneezing, coughing, lifting heavy objects. It is due to nerve and muscle weakness. The prevalence of stress incontinence is not known exactly due to studies in different societies. The rates for women are quite striking. While the prevalence is between 12-52% in women who have never given birth, this rate varies between 4.5-53% in the general population. Pregnancy and vaginal delivery are important causes of female stress incontinence. Other factors depend on gender, race, anatomical structure and familial causes. Causes such as body mass increase, obesity, diabetes and aging are also risk factors for stress incontinence.
- Sudden incontinence: Here, the patient suddenly urinates and leaks urine uncontrollably. There is uncontrolled contraction of the bladder. The most important reason is the inconsistency between bladder muscles and neural stimulation. Some diseases can also cause this condition. These causes include diseases that cause damage to the nervous system, such as diabetes, Parkinson’s disease, and multiple sclerosis.
- Mixed Type: Both conditions are seen together.
- Continuous Urinary Incontinence: In this type, the patient has a constant sense of urine. A constant urinary incontinence is seen, different from the person’s position and time. Frequent surgical procedures or radiotherapy can cause this condition.
- Overflow Type Incontinence: This is seen when the storage capacity of the urinary bladder is exceeded. It can be seen in cases where the feeling of urine is not fully formed in the patient. In this case, the urine reserve is suddenly filled and the patient begins to leak urine. In order to avoid such a situation, the urinary bladder should be emptied at frequent intervals. However, since it is difficult to achieve this during night sleep, urinary incontinence may occur.
What Are The Risk Factors For Urinary Incontinence?
The conditions listed below are among the risk factors for urinary incontinence:
- Advanced age
- Menopause
- Pregnancy
- Normal birth
- Difficult birth
- Baby larger than normal
- Obesity
- Cigarette
- Chronic constipation
- Genetic predisposition
How Is Incontinence Diagnosed?
Some methods are used in the diagnosis of urinary incontinence. We can list these methods as follows:
- Cystometry: This diagnostic method, also known as cystometrogram, is used to measure the pressure in the bladder. While the patient is asked to perform certain maneuvers during the procedure, sterile water is supplied to the bladder via a catheter.
- EMG (Nerve Measurement Test): This diagnostic method is used to see the strength of the nerves that support the muscles with the function of voluntarily holding urine and whether the muscles are in the required position.
- Pelvic Ultrasound: It is a radiological examination that uses sound waves to view the shape and placement of organs in the pelvis.
- Post-Void Residual Study: It is a diagnostic method used to determine how much urine is left in the bladder after urination.
- Urinalysis: It is the method used to eliminate urinary tract infections with similar findings as urinary incontinence.
- Cystoscopy: It is a diagnostic method used to examine the internal structures of the urethra.
What Are Urinary Incontinence Treatment Methods?
Urinary incontinence treatment is carried out with surgical and non-surgical methods, even with drugs.
In the treatment of urinary incontinence, the type of urinary incontinence is decisive for the treatment method.
For example, surgical methods are usually used in stress urinary incontinence, while drug treatment is applied in urge urinary incontinence.
If we open the surgical method a little more, we can say that in this type of surgery, which is usually performed using the external genitalia, the abdomen is not entered.
At this stage, a sling is placed at the exit of the urinary excretory canal to support the area.
Thus, the patient becomes better able to hold his urine.
In the case of urge urinary incontinence, along with the anti-contraction drug treatment, it is also recommended to strengthen the pelvic muscles.
In this direction, kegel exercises that can strengthen the muscles provide benefits to the patient, regardless of what type of urinary incontinence.
Kegel exercises, while tightening the vaginal tissue in women, prevent sagging in the pelvic and female genital organs and allow better retention of urine.
Finally, in some patients with urinary incontinence, positive results can be obtained with muscle-strengthening exercises without the need for surgery or medication.
After the patient is taught what must be used during exercise, the patient is followed up for periods of 3-6 months or 1 year.
Thus, a significant increase in the recovery rate of patients is achieved.
What Are Urinary Incontinence Drugs?
Urinary incontinence drugs are not used in the treatment of all types of urinary incontinence.
Medicines are especially effective in urge urinary incontinence.
In stress incontinence, the desired response cannot be obtained from drug therapy.
However, this situation is slightly different in female patients.
Medication may be preferred in female patients with mixed urinary incontinence.
The drugs of choice in this treatment process are anticholinergic drugs.
With the help of drugs, the detrusor muscle in the bladder does not contract involuntarily.
As a result, the patient does not develop a sudden need to void.
However, no drug should be used unconsciously unless the physician recommends it.
Indiscriminate use of drugs can worsen the condition and cause some undesirable side effects.
The drugs used in the treatment of urinary incontinence are as follows:
- Oxybutynin
- Tolterodine
- Trospium
- Solifenacin
- Darifenacin
- Fosterodine
- Mirabegron
- Imipramine
How To Treat Stress Incontinence In Women?
There are surgical treatment options as well as non-surgical treatments for urinary incontinence in women.
Non-Surgical Incontinence Treatment Methods
Behavioral treatments are at the forefront among non-surgical treatments.
Behavioral treatments include weight loss, smoking cessation, bladder training, lifestyle changes, and balancing fluid intake.
Obesity, in particular, can cause urinary incontinence.
Therefore, losing weight in a balanced way provides improvement in incontinence.
Another non-surgical treatment is pelvic floor rehabilitation.
Involuntary relaxation movements in the muscle structure can be prevented with pelvic floor exercises.
PTE can be applied as initial therapy in incontinence.
Drug treatment for urinary incontinence can be applied in cases where surgery is not preferred.
It is aimed to increase the closing pressure by increasing the urethral passive tone with estrogen therapy.
For this purpose, help can be obtained from estrogen creams, alpha agonists and beta agonists.
Imipramine, on the other hand, is more effective in urge urinary incontinence.
Beta-antagonists increase norepinephrine level and urethral resistance.
However, in this case, side effects such as hypertension, arrhythmia, angina and migraine can be seen.
The last type of non-surgical treatment is vaginal or urethral plug devices.
However, they are less recommended than pelvic floor rehabilitation treatments.
It is recommended for people who are prepared to use vaginal or urethral plugs, who are elderly and who cannot undergo surgical operation.
Surgical Incontinence Treatment
It is possible to apply to injection treatments within the scope of surgical treatment.
In this way, periurethral filling materials are injected into the bladder neck.
With this, coaptation of the bladder length is aimed.
Injection of filling materials under the urethral mucosa into the bladder neck should continue until complete closure is achieved.
This treatment is very advantageous compared to other treatments in terms of its quick applicability, patient tolerance and no need for anesthesia.
However, it is a disadvantageous treatment in terms of cost and effectiveness.
Reapplication may be required, especially since success is short-lived.
In this regard, it is a type of treatment that can be preferred in elderly patients with a high risk of anesthesia.
However, patients should be informed that filling materials will decrease over time, re-injection will be required, and despite these, the chance of success is less than other surgical treatments.
Burch surgery, on the other hand, is today considered the gold standard in the treatment of urinary incontinence.
Autologous sling surgery can be applied to people with severe urinary incontinence.
Apart from this, it can be applied to people who have undergone mid-urethral sling surgery and have unsuccessful results, to patients with a pregnancy plan, and to patients with vaginal fistula.
Autologous sling surgery, like Burch surgery, is a gold standard treatment.
Both treatments have as much chance as primary surgical treatment.
What Is Good For Urinary Incontinence?
There are several methods that can be applied to prevent urinary incontinence.
The first of these is balancing and reducing daily fluid intake.
Especially people who consume beverages such as coffee and tea frequently during the day should pay attention to their amount.
Obesity and weight problems are also among the most important problems that cause urinary incontinence.
For this reason, the person should get rid of excess weight and lose weight.
Although there are some herbal treatment methods that can be applied for urinary incontinence, these are insufficient to provide a permanent solution.
Therefore, the most important thing to do is to see a doctor.
While most people see incontinence as a normal condition as they get older, this is not true.
There are also treatment options for urinary incontinence due to old age.
The doctor will make the appropriate diagnosis for the relevant treatment method.
After the diagnosis is made, the necessary treatment can be started.
What Are Urinary Incontinence Exercises?
Urinary incontinence exercises can be helped to strengthen the pelvic floor muscles.
These muscles are the levator ani muscle, the external anal sphincter, and the striated urethral sphincter muscles.
If these muscles are strong and robust, urinary incontinence is usually not seen.
Urinary incontinence exercises can be done to strengthen these muscles.
These exercises also help reduce stress incontinence by raising the bladder neck.
With the urinary incontinence exercise, also known as Kegel Exercise, the pelvic floor muscles are contracted for 10 seconds and relaxed for 10 seconds.
These movements are applied 20 times and in 3 sets.
Performing these exercises at least 3-4 times a week strengthens the muscles significantly.
The effects of exercise show themselves 2 weeks after starting to do it regularly.
After an average of 3 months, the patient notices a significant reduction in urinary incontinence.
However, in order for the relevant exercise to be effective and successful, the movements must be performed correctly and regularly.
Frequently Asked Questions About Urinary Incontinence
How Is Urine Held?
The bladder, urethra and pelvic floor must be healthy and sound both anatomically and neurologically in order to hold urine.
If there is a problem in any of these, urinary incontinence problem is seen.
The detrusor muscles in the bladder help hold and expel urine.
These muscles work involuntarily.
In the case of contraction of the muscles, the need to urinate is needed, while the feeling of urination disappears if they do not contract.
In order to hold the urine, the integrity between the bladder, bladder length and urethra should not be disturbed.
In order to ensure this integrity, the pelvic floor muscles that hold the relevant organs where they should be should also be strong.
If there is a problem with any of these, urinary incontinence is seen.
Which Herbs Can Be Used For Herbal Treatment of Urinary Incontinence?
Some herbs are beneficial for urinary incontinence.
However, plant selection should be done carefully before trying to apply the treatment.
Since some herbs have a diuretic effect, this treatment should not be applied by people who do not have knowledge of treatment.
Using herbs that do not have a diuretic effect can be beneficial.
However, it should be noted that no herbal remedy alone cures.
Herbal treatments should be applied in addition to the standard treatment.
Herbal cures should not be the main treatment, but supportive treatment.
Plants that may be useful in the treatment of urinary incontinence are as follows:
- Plantain leaf
- Ponytail
- Fennel
- Cinnamon
Herbal mix (Rosemary, yarrow, rhododendron, potentila root)
What Are The Risks Of Urinary Incontinence Surgery?
As with all surgeries, urinary incontinence surgery has its own risks.
The operation should be performed by an experienced surgeon with the correct technique.
It is also important that the treatment plan is chosen correctly.
After paying attention to the relevant points, the risks of the surgery are significantly reduced.
However, in some cases, the following conditions may occur after surgery:
- Inability to urinate
- Continuing urinary incontinence
- Bladder and urethra injury
- Vascular injuries
- Bleeding
- Mesh infection
- Urinary tract infection
- Anesthesia-related risks
Surgery for urinary incontinence usually does not involve many risks.
However, they do carry risks.
Therefore, it should be considered thoroughly before surgery is the first option for the treatment of urinary incontinence.
If the patient is suitable, primarily behavioral treatments, pelvic floor exercises and drug treatments should be preferred.
Surgery can be recommended for patients who do not see improvement even after the implementation of all these.
What Is Fecal Incontinence?
Fecal incontinence is the loss of control of bowel movements.
As a result of losing control of bowel movements, the problem of gas and stool leaking through the anus arises.
Gas can cause a more severe loss of control over liquid or stool.
This is a fairly common problem that 1 in 10 people may face in their lifetime.
Especially not being able to reach the toilet quickly can cause leakage and intestinal accidents.
This situation is quite uncomfortable for the patient and can significantly affect the person’s daily life.
Many people who have this problem are hesitant to explain the situation to doctors and nurses.
People are especially embarrassed when their family and friends know about this situation.
However, this is a wrong attitude.
If a doctor is examined without wasting time, treatments can be applied to help improve this problem.
See also: Lifestyle Changes To Help You Lower Blood Pressure
